Osteoporosis and Osteopenia are very common especially in women over the age of 60. There are a lot of reasons for osteoporosis and often times there is a genetic component. Sometimes you can do everything right and the process continues despite all your efforts.
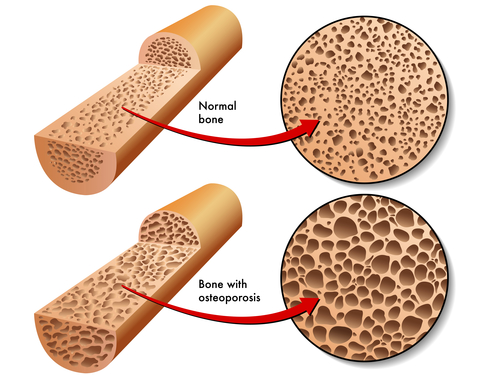
The basic reason for bone loss is an uncoordinated bone remodeling process. It is a signaling mechanism between the bone forming cells called osteoblasts and the osteoclasts, which are responsible for absorbing bone tissue during growth and healing.
This interaction is a fine balance but as we get older our bones develop more micro fractures so this signaling gets ramped up and it increases osteoclastic activity.
As the skeletal structure continues to weaken the body is always attempting to strengthen it.
As our bodies generally become more inflamed when we get older creating more cytokines or inflammatory messengers this will increase the osteoclast activity. During this inflammatory phase they also become much more aggressive and they begin to break down bone even more.
Therefore when addressing osteoporosis it is imperative that a Functional Medicine approach be taken to evaluate the whole body and identify the imbalances. This would include the gut, thyroid, pancreas, and reproductive organs. The goal is to minimize inflammation and reduce these pro-inflammatory cytokines.
The inflammatory state as stated accelerates the production of osteoclasts causing more bone absorption.
Within a standard blood test we can look at a few markers such as the red blood cell count. With individuals that have osteoporosis this count is generally below 4. This is because instead of increasing osteoblastic activity the body will switch to a more fat producing mode within the bone marrow affecting stem cell production of the red blood cells. Also, the mean platelet volume (MPV), can suggest an inflammatory process.
This process of more inflammation within the body, increasing bone resorption and decreasing the production of more bone growth will continue unless the inflammatory process is corrected.
It is not quite as simple as providing calcium or exercising but rather improving the communication between the bone forming cells and bone resorption cells.
Genetics plays a part due to the fact the genes control vitamin D production and Collagen. However, what we have learned about genetics is they can be turned on and off or supported to assist them in their function. When I address a patient I tend to look at genetics and markers for vitamin D such as the VDR.
The other component we want to measure is bone quantity and bone quality.
We evaluate DEXA and T scores and look at the numbers. For example if a person has a -3.5 I begin to get a bit more nervous and realize the time to improve this is much more narrow than perhaps a -2.0. I am not opposed to the bisphosphonates; I just believe they are over prescribed and not addressing the root of the problem.
Also, I like a urine test call N-teleopeptide to look a bit closer at bone resorption and to establish a base line to make sure the treatment protocols recommended are actually working. The reference range is 15-60, which is a huge range. Ideally, we would want a patient to be around 30-45. If it were too low there would be no bone remodeling and have a higher risk for fracture.
If the marker is high our goal is too get this down below 50 in 3-6 months with proper nutrition. If this does not work we recommend working with you Doctor and discuss the use of medications.
With some patients their numbers on their DEXA scan are so bad they need to be on medications immediately.
Nutrition will work but sometimes the benefits to risk ratio must be assessed and determine if the slower process of proper nutrition is suitable for this patient given all the factors.
Some of the drugs like Forteo will actually build bone and tissue. At times I will recommend this with a bisphosphonate and then after a period of time eliminate the bisphosphonate and just provide the nutrition.
Of course we are constantly monitoring the bone resorption markers.
Our nutrition program consists of Vitamin D. I like to see their numbers around 50-70. I also recommend K2, MK4 and MK7. Minerals such as calcium, magnesium, as well as trace minerals. For remodeling I utilize alpha lipoic acid and NAC. Berberine helps to decrease osteoclastic activity and increase osteoblastic activity. Taurine has been proven to stimulate osteoblast activity. Lastly, I recommend medium chain triglycerides like Coconut Oil.
Often times these individuals are protein deficient so I recommend increasing protein intake or even an amino acid supplement.
When dealing with Osteoporosis we must keep in mind that it is important to have a whole body approach. Just taking calcium and exercising is not going to have that great of an impact on your results. Also, the labs to help monitor your progress are important to measure success. If conservative treatment does not work there are medications that can be effective.

